June 11, 2020
Innovative Technologies towards building Affordable and equitable global Radiotherapy capacity (ITAR)
A new project, “Innovative Technologies towards building Affordable and equitable global Radiotherapy capacity” (ITAR), supported by the Science and Technology Facilities Council (STFC), aims to design and develop new radiotherapy technologies to give more cancer patients in Sub-Saharan Africa access to treatment and to save lives. The project will contribute to the development of novel radiotherapy machines, specifically designed to meet the needs of African hospitals. The challenge brings together an international team of accelerator physicists and engineers, medical physicists, radiobiologists, radiation oncologists, radiologists, IT experts, and health system researchers.
The state of cancer care
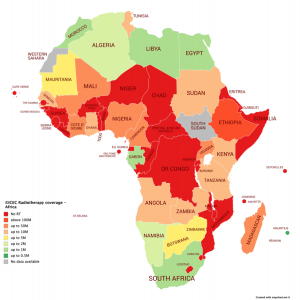
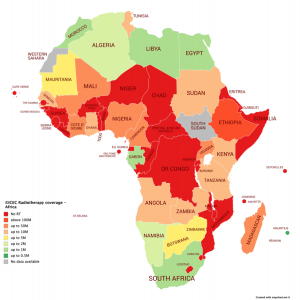
The number of people per radiotherapy machine per African country
The annual global incidence of cancer is projected to rise to 27.5 million cases by 2040, leading to more than 13 million deaths. Up to 70 percent of these will occur in low and middle-income countries (LMICs). Radiotherapy is an essential component of cancer care being a very effective means of curing the disease, as well as palliative treatment, and where available, is used to treat more than half of patients.
Many low and middle-income countries in Africa have acute shortages of radiotherapy machines. In the lowest-income countries, only four percent of cancer patients that need radiotherapy treatment are able to be treated. There are currently only 385 radiotherapy machines in the region, and 60 percent of those are located in just three countries – South Africa, Egypt and Morocco.
A report by the Lancet Oncology Commission – Global Task Force on Radiotherapy for Cancer Control (GTFRCC) of the Union for International Cancer Control (UICC) recently estimated that by 2035 at least 5,000 additional megavolt-class treatment machines would be needed to meet radiotherapy demands in low-and middle-income African countries.
A collaborative effort
The ITAR project, a critical part of a larger international project that includes the International Cancer Expert Corps (ICEC), CERN, STFC (Daresbury Laboratory), and Lancaster University, is led by Lancaster University and Oxford University and will bring together partners from the Cockcroft Institute, STFC’s Accelerator Science and Technology Centre (ASTeC), John Adams Institute, Swansea University, King’s College London, ICEC and CERN.
In ITAR’s first phase, the project will define the persistent shortfalls in basic infrastructure, equipment and specialist workforce which remain barriers to effective radiotherapy delivery, and develop novel solutions leading to a detailed specification and conceptual design. The project will then progress to a prototype development phase at STFC’s Daresbury Laboratory.
Professor Manjit Dosanjh, from CERN and Oxford University, and member of the ICEC Board of Directors, and who leads the overall international project, said: “I am really excited that the idea, first presented by Dr Norman Coleman of the International Cancer Expert Corps at the 2014 ICTR-PHE meeting held in Geneva, continues to flourish. Having Lancaster and Oxford Universities, along with Daresbury Laboratory and others working on this with STFC’s critical support and ICEC’s expertise, is a significant step in addressing the need for a novel medical linear particle accelerator to generate the radiation for LMICs and other challenging environments.”
Local stakeholder participation is vital to the project’s success

Dr. Taofeeq Ige (National Hospital Abuja, Nigeria) in front of one of the hospital’s radiotherapy LINACs.
A critical aspect of the project’s challenge cluster is the involvement of the international partners. Dr. Taofeeq Ige and Dr. Simeon Aruah, of the National Hospital Abuja, Nigeria, and Dr. Surbhi Grover, of the Botswana-UPENN Partnership and Princess Marina Hospital, are key partners working in African hospitals. They will gather information from a network of other hospitals in Botswana, Ghana, Kenya, Nigeria, South Africa, Tanzania, Zambia and Zimbabwe and play a key role in the definition of the specification for the new machines.
In addition, ICEC provides a network of international oncologists, medical physicists, and engineers working in radiotherapy systems. They are already providing training and mentorship in lower- and middle-income countries and will continue with their assistance in the development of the radiotherapy system in this project.
Professor Graeme Burt, of Lancaster University and the Cockcroft Institute, and who is leading the phase 1 project said: “Current radiotherapy machines are optimised for use in western countries. The ITAR project aims to design specifically for use in Africa making it far more tolerant to the local environment, which will greatly increase the capacity for more lives to be saved.”
Professor Deepa Angal-Kalinin, of STFC and the Cockcroft Institute, University of Manchester, and who is leading the accelerator design said: “I am keen to apply the knowledge and expertise at Daresbury Laboratory to develop a novel medical linac design in this phase of the project which will prepare us to build a prototype to test our novel ideas.”
Media queries should be sent to:
nina.wendling@iceccancer.org or graeme.burt@cockcroft.ac.uk